Vision rehabilitation using microperimetric biofeedback training in age-related macular degeneration
Sri Hudaya Widihastha, Erwin Iskandar, Karmelita Satari, Irawati Irfani, Rova Virgana,Primawita Oktarima Amiruddin
1Department of Ophthalmology, Faculty of Medicine,Universitas Padjadjaran, Bandung 40117, Indonesia
2National Eye Center Cicendo Hospital, Bandung 40117, Indonesia
Abstract● AIM: To determine the impact of microperimetric biofeedback training (MBFT) on the quality of vision in patients with age-related macular degeneration (AMD).
● KEYWORDS: microperimetric biofeedback training; agerelated macular degeneration; vision rehabilitation
INTRODUCTION
Age-related macular degeneration (AMD) is a degenerative disease affecting retinal tissue that may cause central vision loss and occur in people over 50y.AMD accounts for 8.7% of total blindness worldwide, and it is the most common cause of blindness in developed countries in people over 60y.It also accounts for a 5.64% prevalence of people with moderate to severe visual impairment[1-3].The World Report on Vision has reported that the estimated population of AMD patients worldwide in 2020 is 196 million.This figure is expected to increase, with the projected number of AMD prevalence in 2040 reaching 288 million[4].The total population of Asia,which covers more than 60% of the world’s population, will experience the largest projected number of AMD cases, with an estimated one-third of cases globally, although for now,Europe has the highest prevalence of AMD, which is 11%[5].
A person with central visual field impairment tends to experience adaptive mechanisms to improve visual performance by creating a new preferred retinal locus (PRL) or “pseudofovea”[6-7].Microperimetry is an examination tool used to assess retinal sensitivity in a non-invasive and computerized manner and assess fixation stability and digital fundus photography in one instrument[8-10].This microperimetric examination can also be utilized to assess the preferred retinal locus shift in patients with macular disorders.Microperimetry has a microperimetric biofeedback training (MBFT) module that can train patients who have lost foveal fixation to relocate the locus to an area with greater sensitivity.Several studies have researched the benefits of MBFT and showed promising results[11-14].
To date, standard practice consensus regarding the required frequency and number of sessions is not applicable.Therefore,this study aimed to examine the impact of MBFT on visual acuity, near vision acuity (NVA), fixation stability, and reading rate in patients with AMD.
SUBJECTS AND METHODS
Ethical Approval The study was performed according to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of National Eye Center Cicendo Eye Hospital, Indonesia with registration number LB.02.01/2.3/039/2021.
This study was a single-center prospective, comparative study of patients diagnosed with AMD who came to the National Eye Center (PMN) Cicendo Eye Hospital as subjects between March and June 2022.The subjects were randomly divided into two groups, the intervention group and the non-intervention group, with balance block randomization.The inclusion criteria in this study were: 1) Patients diagnosed with AMD confirmed based on funduscopy and macular optical coherence tomography (OCT) examination, with best corrected visual acuity (BCVA) of more than 1/60 and less than 0.3 logMAR.If the patient has bilateral AMD, the eye with worse visual acuity was selected; 2) No indication for anti-vascular endothelial growth factor (VEGF) therapy; 3) The patient agreed to be trained.The exclusion criteria include: 1) Patients who have impaired hearing function, physical limitations, and cognitive impairments; 2) Other eye diseases such as glaucoma, optic nerve disorders, and history of intraocular surgery other than cataracts; 3) Significant refractive media opacities such as corneal opacities, cataracts, or vitreous disorders that will interfere with training.The drop-out criteria were: 1) Skipping the exercise twice in a row during the training; 2) Not willing to carry on training; 3) A significant change in visual acuity due to worsening of AMD, which macular OCT confirmed.BCVA was measured using an Early Treatment Diabetic Retinopathy Study (ETDRS) chart and was converted into logMAR notation for statistical analysis.Macular sensitivity and fixation stability were assessed using an MP-3 microperimeter(MP-3, Nidek Technologies’).This tool provided a 45° nonmydriatic view of the fundus.The microperimetry examination was conducted under dim-light conditions, with a background luminance of 10 cd/m2and a maximum stimulus intensity of 125 cd/m2.Mean central sensitivity and the mean sensitivity within a 2° radius from fixation were documented before and after intervention using a 4–2 thresholding strategy with the Goldmann III pattern.The retinal light threshold was evaluated using the Goldmann III with stimulus intensity ranging from 0 to 34 dB and a stimulus duration of 200ms.The evaluation result would serve as a guide in training.
In the intervention group, MBFT was performed six times with an interval of one week for ten minutes each session.Meanwhile, the non-intervention group underwent two times of training with an interval of one month.Moreover, we selected the superior and right side of the macula as the new trained retinal locus (TRL).The BCVA, NVA, and reading speed (words/min) were subsequently evaluated and compared between the two groups.
Data analysis included descriptive analysis and hypothesis testing.The statistical analysis began by conducting a homogeneity test of characteristics in both groups to see the feasibility of the two groups being compared.Next, the Chisquare test was utilized to test statistical analysis for categorical data.Before carrying out statistical tests on numerical data, it was first assessed by a normality test using the Shapiro-Wilk test.The significance test used to compare the characteristics of the two groups was the unpairedt-test for normally distributed data and the Mann-Whitney test if the data were not normally distributed.
Furthermore, to analyze the comparison of the mean before and after the intervention, pairedt-test was used if the data were normally distributed or the Wilcoxon test if the data were not normally distributed.The significance of the statistical test results was determined based on theP<0.05.The data obtained were recorded in a special form and then processed with the SPSS version 26.0 for Windows.
RESULTS
A total of 36 eyes from 36 patients diagnosed with AMD were included in this study.There was no drop-out reported during the process.A comparison of the demographic and clinical characteristics of the two groups is listed in Table 1.The results of statistical tests on the variables of age, sex, laterality,thicknesses of central subfield, lens status, BCVA, NVA, and reading rate showed no statistically significant difference in the proportion of the intervention and non-intervention groups.Therefore, the data was considered homogeneous and feasible to compare.
Table 2 compares the results of the BCVA, NVA, fixation stability, and reading rate before and after training in the intervention group.These results show an improvement in BCVA and NVA followed by an increase in reading rate.Based on statistical calculations, BCVA, NVA, and reading rate variables, a statistically significant mean difference was observed among the abovementioned variables before and after training in the intervention group.
Table 3 compares changes in the same three variables between the intervention and non-intervention groups.Statistical tests performed resulted in a statistically significant mean difference between those particular changes.
DISCUSSION
Structural damage to the fovea due to macular disorders can lead to loss of central vision and cause decreased visual acuity.To date, no medical intervention can effectively fully reverse the loss of macular function[13].Therefore, some interventions have been developed to modify the visual system to improve the quality of vision in patients with macular disorders[14-15].MBFT is one of the intervention strategies to train patients to stabilize fixation at the retinal locus with higher sensitivity so that vision improvement can be achieved[16-18].
Amoreet al[18]and Qianet al[19]have demonstrated the use of MP-3 as a rehabilitation program in patients with macular disorders.The former has particularly compared the MBFTeffectiveness of two devices, MP-1 and MP-3, and the results showed no significant difference between them.Furthermore,previous studies conducted by Moraleset al[20], Ratraet al[13],and Ramírez Estudilloet al[21]have reported improved BCVA,NVA, and reading rate after MBFT, specifically in AMD cases.In line with those results, this study also found similar findings before and after visual rehabilitation with MBFT using MP-3.However, Vingoloet al[22]observed different results;improvement in NVA and reading rate was not followed by BCVA.
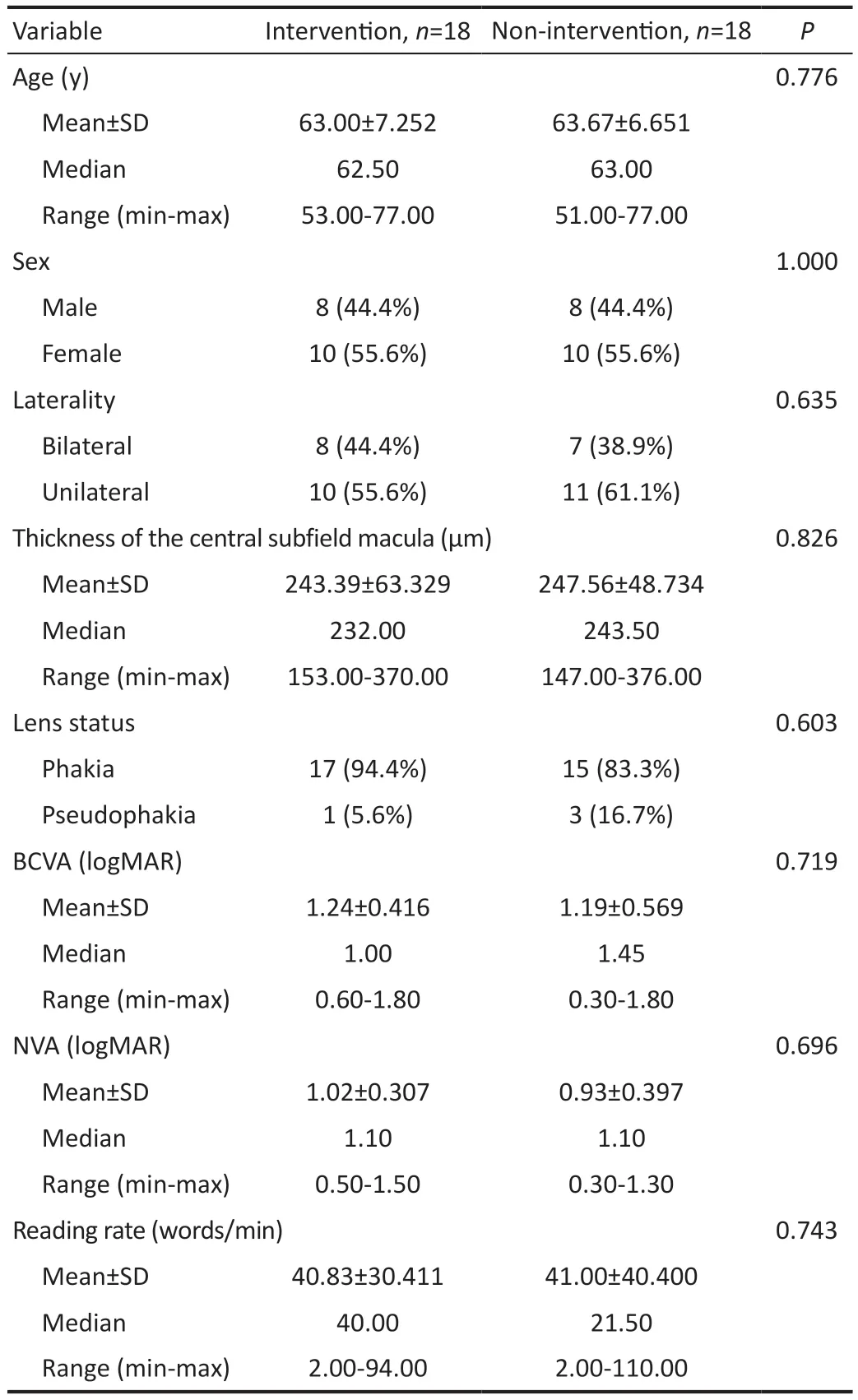
Table 1 Comparison of demographic and clinical characteristics between the intervention and non-intervention groups before MBFT
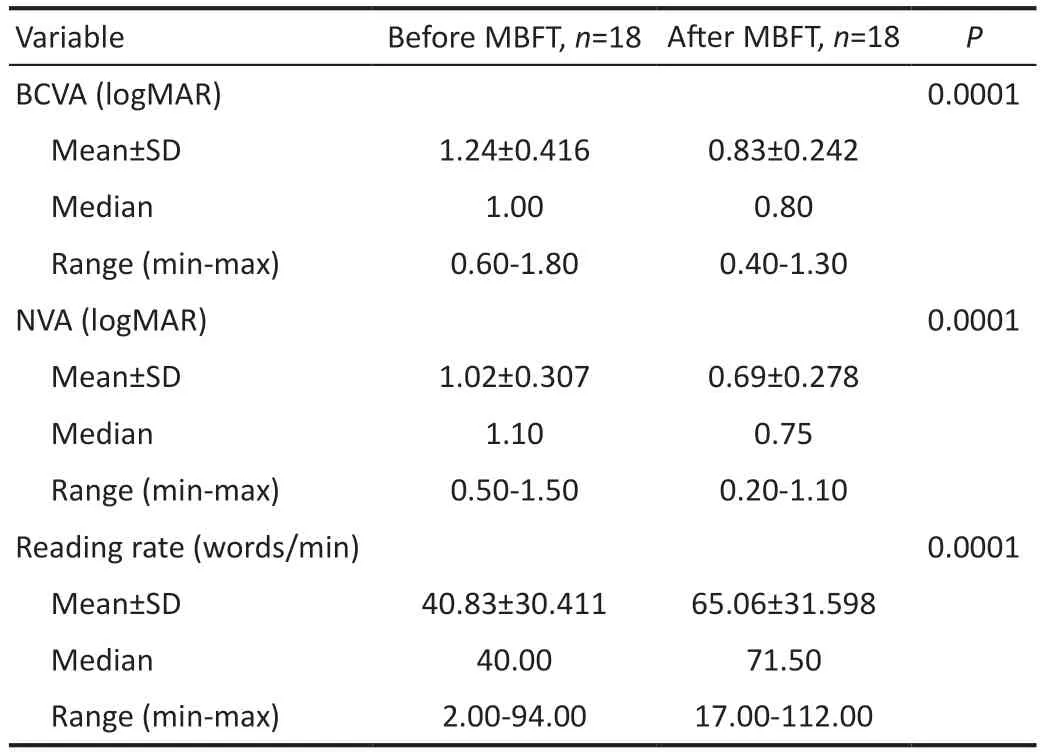
Table 2 Comparison of BCVA, NVA, and reading rate before and after MBFT in the intervention group
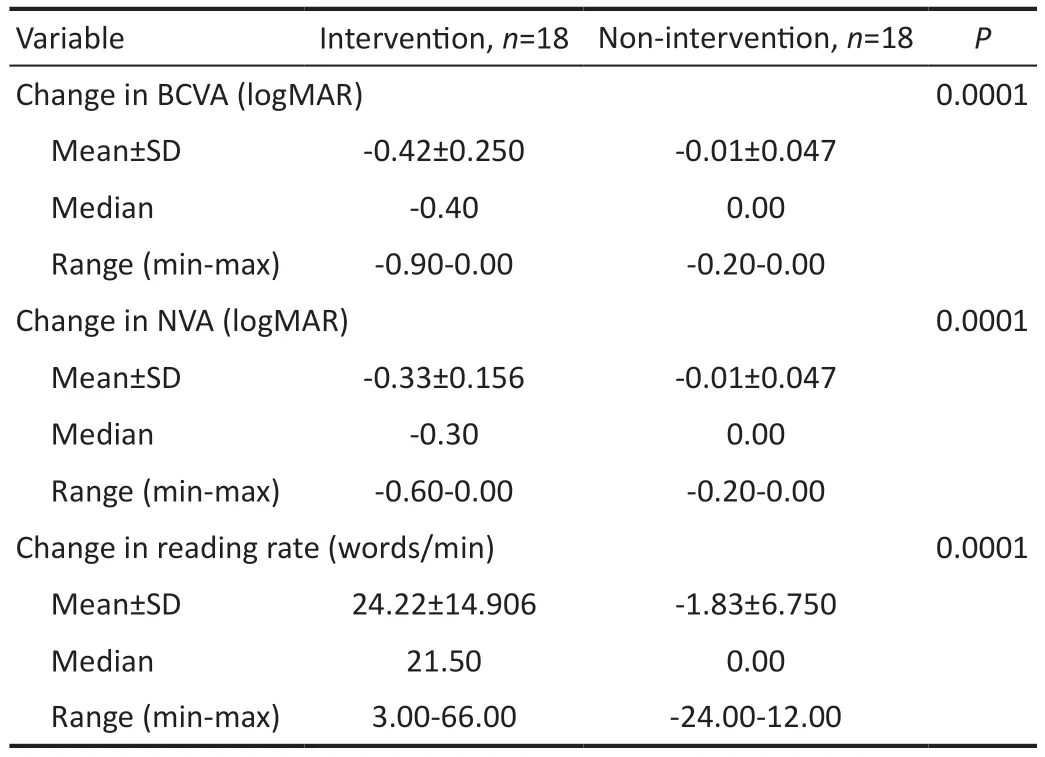
Table 3 Comparison of changes in BCVA, NVA, and reading rate between the intervention and non-intervention groups
Visual rehabilitation using MBFT has been found to improve retinal sensitivity in five different macular diseases[19-25].When an area of the retina is damaged, the activity of cortical neurons there will remain active with stimulation from other parts of the retina[26].MBFT, combined with audio feedback,can help maintain target retinal stimulation, amplifying the patient’s cortical plasticity and facilitating neural signaling to the retina, the retina, and the brain, a phenomenon known as“neuro-remapping”[27].In the case of chronic central scotoma in irreversible macular disorder, adaptation will still occur as the brain will adopt strategies to form alternative fixations with better visual function.However, this process is lengthy and unpredictable, so MBFT aims to shorten its duration and increase its predictability[28].
Another mechanism predicted to improve visual acuity is“biofeedback”.During the training, the eye movements were monitored by the device and followed by audio feedback generated to signal whether the patient’s fixation was appropriate.Thus, this will help the patient transfer fixation from the degenerated central macular area to a nearby healthy area accompanied by reorganizing the primary visual cortex[28].The reorganization process of the visual cortex has been reported to occur naturally, demonstrated by functional magnetic resonance imaging studies in pediatric patients with foveal vision loss.Some patients with foveal damage will use the extrafoveal area of the retina as compensation over six months[29].This condition is also called eccentric fixation, and the eccentric area of the peripheral macula selected for fixation is called the PRL[19].Shimaet al[26]claimed that PRL was not always the area with the highest sensitivity.Therefore, the concept of a TRL was developed, where the location of the retinal locus can be chosen in the area closest to the fovea, and the area with the highest retinal sensitivity will provide better visual acuity.Microperimetric examination gives information on healthy retinal areas so that patients can identify and practice fixation optimally[23-26].
MBFT techniques can be done by increasing the fixation stability on the already formed PRL or selecting a new TRL as the new fixation point[25].Several studies have shown that these two techniques have the same effectiveness in improving the quality of vision[17].The results of research conducted by Sharmaet al[27]reported improvements in retinal sensitivity after TRL training, persisting up to 1y after exercise.In another study, Vingoloet al[22]performed PRL training on AMD patients and showed significant improvements in font size and reading speed.However, there was no statistically significant change in BCVA.
In this study, we performed MBFT by selecting a new TRL and training the patients for fixation at the new locus.TRL in the superior area and to the right of the fovea was selected,leading to good rehabilitation results and increased BCVA,NVA, and reading rates.Many studies have shown that most of the PRL detected in patients with AMD occurs in the retinal superior or right quadrant, which corresponds to the inferior and left portions of the visual field[22-23].Selecting these particular TRL areas showed good rehabilitation results.The superior area related to the inferior visual field is considered important for reading and other near-daily activities.The strong tendency for retinal locus formation on the right side is due to its positive effect on reading performance.For leftto-right reading activities, patients can estimate the amplitude of eye movements to the next word.The retinal locus at this location can result in better reading performance[25,27].
In several studies related to MBFT, reading ability is one of the clinical predictors for evaluating visual function[17].Reading ability can be measured through NVA and reading speed.Any improvement in reading speed may reflect an improvement in visual function in those with maculopathic disorders.Patients with central scotoma will experience a dramatic decrease in reading performance[30-31].Several studies have also shown a significant correlation between reading speed and quality of life[17].Therefore, one of the goals of visual rehabilitation should be to help patients to read again or improve their reading performance.As shown in this study’s findings, MBFT showed a promising result in improving reading speed.
Giacomelliet al[31]demonstrated that several factors could limit reading ability, including fixation instability and reduced contrast sensitivity.Patients with macular disorders will experience decreased visual acuity, contrast sensitivity, and color perception accompanied by a central scotoma in the visual field, which will interfere with their reading ability.
Differences in intensity, frequency, and duration of training in different studies can also provide different rehabilitation outcomes.Until now, research that aims to determine the most optimal MBFT protocol is still being carried out.In most studies, the MBFT program consisted of 10 sessions of 10min each, although a number of sessions ranging from 3 to 16 have been reported in the literature[17].Several research results,including Vingoloet al[22], noted improvements in visual acuity and reading rate in 15 AMD patients who underwent bilateral MBFT with an MP-1 device after ten sessions of 10min each week.They also claimed that visual performance could be maintained by performing five follow-up training sessions every three months.Tarita-Nistoret al[32]also performed MBFT using an MP-1 device for five sessions lasting 1h to relocate the PRL and reported improved fixation stability and better reading performance.However, Sharmaet al[27],performing MBFT 10 times within 10min on both eyes with myopic maculopathy, showed different results where the visual acuity (VA) did not change after exercise; only retinal sensitivity and fixation stability were improved.The most extensive study with the longest follow-up using MP-1 was performed by Silvestriet al[17]and reported results for 171 eyes of 99 patients.This study conducted 16 TRL training sessions and showed an increase in VA in 76% of patients, but 19.2%experienced a decrease in VA after 12mo.In this study, six times of training with one-week intervals and 10min duration each session were carried out.With a total number of training exercises less than in other studies, it is hoped that this study can be used as a baseline for the standard given to patients with AMD.
Although it looks promising, the duration effect of MBFT on visual quality remained vague.Ratraet al[13]reported a follow-up effect of up to 6mo and found a slight decrease in fixation stability.Sharmaet al[27]observed an increase in fixation stability and retinal sensitivity after TRL training and even persisted up to 1-year follow-up, suggesting that MBFT provides permanent results through a remapping mechanism between retinal and brain neurons.Moraleset al[20]showed a slight decrease in fixation stability parameters after three months and suggested that training for a longer time is required to achieve permanent results.In this study, we did not perform long-term follow-up.Considering AMD pathophysiology, which can deteriorate,the possibility of a change in the training effect certainly cannot be avoided.This might be a consideration for providing repeated follow-up training and reviewing the patient’s retinal sensitivity.
The limitations of this study include the absence of an assessment of the long-term effects of rehabilitation.Further research to investigate the long-term effectiveness of MBFT is needed, especially in the setting of progressive macular disorders.In addition, we did not identify the size of the macular scar; thus, we could not compare the degree of macular disturbance in our study and other studies.Skipping regular macular OCT examinations also contributes to unidentifiable anatomical changes to the macula during the training process.Despite these limitations, the study results are expected to form the basis for larger-scale controlled clinical trials in the future.
In conclusion, MBFT is a non-invasive therapeutic approach that significantly and positively impacts visual acuity, near vision acuity, and reading rate in patients with AMD.The present data also highlights that this vision rehabilitation technique has potential to be combined with standardized treatments to promote visual function in patients with disorders affecting the central vision.
ACKNOWLEDGEMENTS
Conflicts of Interest:Widihastha SH, None; Iskandar E,None; Satari K, None; Irfani I, None; Virgana R, None;Amiruddin PO, None.
 International Journal of Ophthalmology2023年6期
International Journal of Ophthalmology2023年6期
- International Journal of Ophthalmology的其它文章
- Preliminary proteomic analysis of human tears in lacrimal adenoid cystic carcinoma and pleomorphic adenoma
- Assessment of the effects of intrastromal injection of adipose-derived stem cells in keratoconus patients
- Evaluation of optic nerve head vessels density changes after phacoemulsification cataract surgery using optical coherence tomography angiography
- Stability of neodymium:YAG laser posterior capsulotomy in eyes with capsular tension rings
- Comparison of the efficacy and safety of ultrasonic cycloplasty vs valve implantation and anti-VEGF for the treatment of fundus disease-related neovascular glaucoma
- Volumetric fluid analysis of fixed monthly anti-VEGF treatment in patients with neovascular age-related macular degeneration
