Acute micro-macular hole associating with extensive intraoperative rotation of implantable collamer lens without ophthalmic viscosurgical device assistance: a case report
Guan-Xing Dang, Yan Li, Xin Zhou, Cong-Yi Wang
Shaanxi Eye Hospital, Xi’an People’s Hospital (Xi’an Fourth Hospital), Affiliated People’s Hospital of Northwest University,Xi’an 710004, Shaanxi Province, China
Dear Editor,
We are writing this letter to report a micro-macular hole (mMH) following the intraoperative rotation of implantable collamer lens (ICL, V4c, Staar Surgical, Monrovia,CA, USA) without ophthalmic viscosurgical device (OVD)assistance and eventually this mMH closed spontaneously.
Due to its safety and efficiency, OVD-free ICL implantation method has become increasingly popular compared with traditional OVD-dependent method for myopia correction.Compared with previously reported cases[1-3], this case presents a strong association between mMH and the surgery method,which eliminates the effect of independence risk factor of high myopia on the formation of macular hole (MH).Meanwhile,basing on the previously reports, we observing this mMH also has the potential to spontaneously close.
CASE PRESENTATION
A 22-year-old female was referred to Xi’an People’s Hospital for the consultation of surgical corrections of her refractive errors.Medical history revealed that she suffered recurrent conjunctivitis caused by contact lens wearing.Upon examination, the corrected distance visual acuity (CDVA) was
16/20 right eye (OD) with a refraction of -9.75 diopters (D)and 16/20 left eye (OS) with a refraction of -10.0 D.The study is followed the Declaration of Helsinki and the patient has given her consent for her images and other clinical information to be reported in the journal.
After the evaluation of the risk of postoperative corneal ectasia, the ICL implantation but not laser vision correction was recommended for the patient.The ICL diameter was determined through the manufacturer recommendations based on anterior chamber depth (ACD) measured with cirrus high definition optical coherence tomography (HD-OCT)and the horizontal white-to-white distance with a cliper.The power calculation was performed using software provided by manufacturer.Corneal endothelial density was measured using SP-3000P corneal endothelial cell counter (Topcon Company,Japan).The fundus examination with macular optical coherence tomography (OCT, Cirrus HD-OCT; Figure 1) and Optos UWF apparatus (Optos Daytona, Optos PLC, Dunfermline, UK)were normal.
We performed OVD-free ICL implantation in the right eye through a 3 mm clear corneal temporal main incisions and a 1 mm side port.With the side port infusion of balanced salt solution (BBS) through a custom-made smooth needle, the 13.2 mm ICL was implanted through temporal incision directly by VISCOJECT eco (Medicel AG, VE2200) to posterior chamber.
On postoperative day 1, the uncorrected distance visual acuity(UDVA) was 16/20, the intraocular pressure (IOP) was 14.5 mm Hg, the vault was 913 μm and the residual ACD was 1.830 mm.No complaints of ocular discomfort were reported.The left eye was operated on the following day with the same size.In order to reduce the danger of angle closure glaucoma,the lens was rotated to vertical orientation intraoperatively.With no OVD assistance, the anterior chamber collapsed twice when the rotation was done by hook through main incision.On the left eye postoperative day 1, the UDVA was 16/20, which was also agreement with the preoperative CDVA, the IOP was 15.7 mm Hg, the vault was 752 μm and residual ACD was 2.048 mm.However, a mild metamorphopsia was noticed by the patient in the left eye in comparison with the right after sequential bilateral surgery.Ophthalmoscopy following pupil dilation revealed a yellow rings in the macular area.The macular OCT examination indicated an mMH in the left eye(Figure 2).
A closely observation approach was taken after communication with the patient since the UDVA in the left eye was not severely affected and an mMH had potential to close spontaneously.After 2mo follow-up, the left eye UDVA was stable at 16/20 and the chief compliant had disappeared.Macular OCT examination revealed that the mMH had closed spontaneously, except the inner segment/outer segment (IS/OS)interface and outer segment of photoreceptor were not entirely intact (Figure 3).Despite the eventful procedure, the patient was satisfied with her visual quality.
DISCUSSION
ICL implantation without OVD assistance is increasingly popular for its outstanding effectiveness and equal safety,which avoiding the postoperative IOP high peak and the safety of not adding additional surgical complications[4].However,there was some reports about MH occurrence following ICL implantation[1-3].
It should be noted that these MHs didn’t present immediately after surgery, but instead showed up several months later.Because of the independent risk factor of high myopia[5]and disease-free interval from ICL implantation to MH onset, the association between MH and ICL surgery was less evident.Only Junet al[2]reported a case which was an acute postoperative MH resulting from ICL surgery and the author attributed acute MH formation tode novoidiopathic MH that was provoked by anteroposterior traction related to implantation.Although this case could exclude the effect of high myopia independent risk factor on MH formation,the patient received ICL surgery from the other center and MH occurred only in one eye with bilateral toric ICL (TICL)implantation.It was unclear that MH had anything to do with the degree of TICL rotation and the usage of OVD intraoperative.
We report an mMH formation followed by rotation of ICL without OVD to vertical orientation intraoperatively, which in order to eliminate the risk of angle-closure glaucoma[6].In our case, with the help of high-resolution OCT, we observed that an mMH appeared immediately in left eye with sequential bilateral non-TICL implantation without OVD.The only difference was whether the lens was rotated to vertical intraoperatively.For non-TICL, the lens could be rotated to vertical in order to reduce the risk of additional surgery.But when extensive intraoperative rotation of ICL was required, especially the rotation of ICL was done through the main incision by hook, OVD-free method might generate a temporary ocular hypotony which is the resource for mechanical traction on the macular during surgery.This was similar to the pathogenesis suggested by Gass[7]that anteroposterior and/or tangential traction in the premacular vitreous cortex playing the main role for MH formation.
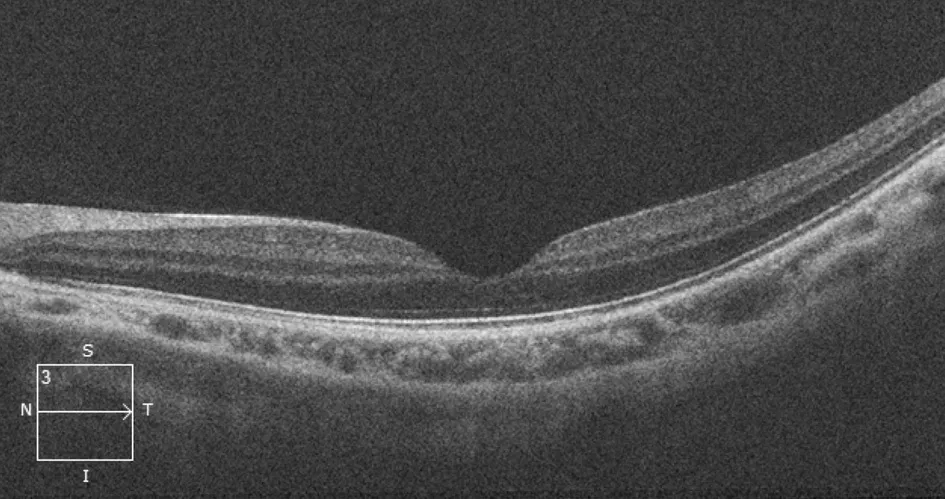
Figure 1 Preoperative macular OCT of the left eye did not reveal any macular abnormalities or vitreous macular traction OCT: Optical coherence tomography.
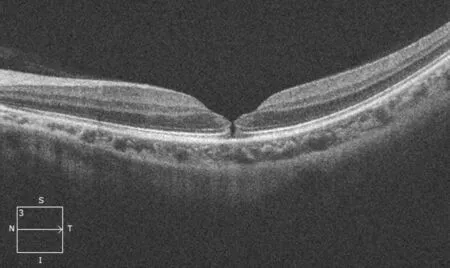
Figure 2 Postoperative 1d of the left eye, OCT shows a full-thickness mMH formation OCT: Optical coherence tomography; mMH: Micromacular hole.

Figure 3 Postoperative 2mo of the left eye, OCT shows slightly residual defects of IS/OS interface and photoreceptor of outer segment OCT: Optical coherence tomography; IS: Inner segment; OS:Outer segment.
Those cases reported before had resorted to surgical treatment eventually.Because our patient’s visual acuity was not severely affected and the MH diameter was quite small, we referred to closely observation.The spontaneous closure nature of MH has been previously reported[8].According to clinical studies, earlier stage and smaller MHs were more likely to spontaneously close.Small MHs have a 15.4% chance of spontaneous closure[9].As well as Uwaydatet al[10]study suggested that it is reasonable to observe recent onset MHs for non-surgical closure, particularly in the setting of blunt ocular trauma.According to increasing evidence, retinal tissue bridgingviaretinal cell proliferation across the MH is the primary cause of spontaneous closure of the MH[11].Morawskiet al[12]observed the closure process of MHs in 10 eyes of 10 patients and indicated that the mechanism of closure was mainly associated with the bridging phenomenon and posterior vitreous detachment that allowing the release of vitreous macular traction was not necessary.
Regeneration of the photoreceptor interface IS/OS was critical to postoperative vision restoration.This bridging phenomenon was confirmed by the spontaneous closure of mMH in our case and the photoreceptor interface IS/OS was nearly intact.This case highlights that although OVD-free ICL implantation has shown to be a safe and effective option, the OVD may play a key role to reduce the risk of MH formation when extensive intraoperative rotation is done through main incision.Micro-MH induced by ICL implantation, like idiopathic ones, can be closely observed in an attempt to minimize the possibility of further surgery.In the future, a large sample size study would be necessary to elucidate the relationship between the MH formation and operation methodology.
ACKNOWLEDGEMENTS
Authors’ contributions:Dang GX collected the preoperative and postoperative data and performed a major contribution to writing the manuscript.Wang CY performed the surgery.Li Y and Zhou X participated and made great effort in reviewing literature sources and writing this manuscript.
Conflicts of Interest: Dang GX,None;Li Y,None;Zhou X,None;Wang CY,None.
 International Journal of Ophthalmology2023年10期
International Journal of Ophthalmology2023年10期
- International Journal of Ophthalmology的其它文章
- A novel approach for 25-gauge transconjunctival sutureless vitrectomy to evaluate vitreous substitutes in rabbits
- Visual resolution under photopic and mesopic conditions in patients with Sj?gren's syndrome
- Effects of obstructive sleep apnea on retinal microvasculature
- Bibliometric analysis of research relating to refractive cataract surgery over a 20-year period: from 2003 to 2022
- Three-dimensional bioprinting in ophthalmic care
- Agreement of intraocular pressure measurement with Corvis ST, non-contact tonometer, and Goldmann applanation tonometer in children with ocular hypertension and related factors
