Management of complex and redo cases of pelvic fracture urethral injuries
Sanjay B.Kulkarni,Sandesh Surana,Devang J.Desai,Hazem Orabi,Subramanian Iyer,Jyotsna Kulkarni,Ajit Dumawat,Pankaj M.Joshi*
Department of Reconstructive Urology,Kulkarni Reconstructive Urology Centre,Pune,India
1.Introduction
Pelvic fracture may lead to urethral injury in about 10%of patients[1].The common site ofinjury is at the bulbomembranous junction.Rarely the site ofinjury in adults may be at the prostate-membranous junction ascompared to children where this is commonly the case.Due to the nature ofinjury,the urinary bladder along with prostate and membranous urethra gets displaced cranially.The aim of surgery is to achieve a tension free bulbo-membranous anastomosis.
Anastomotic urethroplasty remains the gold standard management for pelvic fracture urethral injuries(PFUI).Stepwise elaborated perineal approach is the current preferred option.Transabdominal approach is used in selected cases.We discuss the management of complex PFUI in eight scenarios.
2.Patients and methods
Our institute is a tertiary referral centre for reconstructive urology cases.We retrospectively reviewed our prospective database from January 1995 to May 2016.Five surgeons including Society of Genitourinary Reconstructive Surgeons(GURS)fellows at our institute have performed 1062 surgeries for patients with PFUI.Complex PFUI cases were subdivided into eight groups.Patients were either followed up at our centre or with the referring urologist.Internetbased applications like email and WhatsApp were used to acquire follow-up uroflow and American Urology Association(AUA)symptom score data from patients.
All patients were evaluated prior to surgery with voiding cystourethrography(VCUG)through Suprapubic(SPC)tract and retrograde urethrography(RGU).Patients with recto urethral fistula,double block,false passage and bladder neck injury underwent Magnetic Resonance Imaging(MRI)prior to surgery.
We have developed a new protocol for MRI image acquisition in patients with PFUI[2].We performed MRI with pre-administration of alpha-blocker,keeping a full bladder by clamping the SPC and instilling saline with lubricating jelly in the urethra.Urine in the bladder and saline in urethra act as a natural contrast on T2 weighted image(Fig.1).Images acquired closely resemble traditional VCUG/RGU and are easy to interpret.
Preoperative penile doppler was performed in all male patients>18 years age.Flow velocity in the cavernosal arteries and deep dorsal penile artery was documented prior to and after injection ofintracavernosal papavarine.All patients had an SPC on referral.Intraoperatively urethroscopy was performed to assess penile and bulbar urethra.Antegrade scopy was performed to assess the bladder,bladder neck,prostate and membranous urethra.Occasionally we found co-existent pathology-bladder stones;Retained catheter tip,which required endoscopic management.In all patients tension free anastomosis was performed using 4-0 Polyglactin/5-0 Polydioxanone sutures.Urethral catheter and SPC were kept for 4 weeks postoperatively.Pericatheter VCUG was performed in majority of our patients due to the complexity of reconstruction.In patients with an anastomotic leak the catheter was kept for an additional 2 weeks.
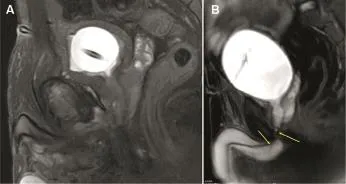
Figure 1 MRI of pelvis with empty bladder(A)and with our protocol with full bladder and jelly in urethra(B).The left arrow means bulbar urethra;The right arrow means the injury is at the level of bulbo membranous junction.
Failure was defined as flow less than 12 mL/s and/or requirement of single postoperative dilatation,visual internal urethrotomy or a repeat urethroplasty.These interventionswereindicatedforsymptomaticand objectively documented poor flow.
3.Results and discussion
We discuss our results in eight categories of complex PFUI.
3.1.Redo cases
Of 1062 PFUI cases,541 were redo cases.Redo cases had undergone up to five prior attempts at anastomotic urethroplasty before being referred to us.The mean age of patients was 28.4 years(8-55 years)and the mean follow-up was 68 months(12-240 months).The overall success rate of redo cases was 79.13%.The success rate was slightly lower but comparable to that of primary cases,which was 85.60%(n=521)over the same period of time(Table 1).
We subclassified PFUI into three categories:primary,one failed urethroplasty,and≥2 failed urethroplasties.
There were three distinct findings in cases of redo PFUI:
1.The scar tissue excision was inadequate.In most cases of previous failed urethroplasty there was an extensive scar that required excision.This scar tissue either prevented identification of normal healthy prostatic urethra or caused constriction resulting in narrowing at the site of bulbomembranous anastomosis.
2.The urethra was not adequately mobilized at prior surgery in 63%of cases(Fig.2A).The bulbar urethra should be mobilised till penoscrotal junction to utilise the inherent elastic lengthening property of bulbar urethra in performing a tension free anastomosis.International ConsultationonUrological Diseases(ICUD)defines bulbar urethra as the urethra that lies within bulbospongiosus muscle.If one mobilizes only this part of the urethra it cannot be stretched adequately.Hence,bulbar urethra should also include the urethra till the penoscrotal junction.Any dissection distal to the penoscrotal junction may result in chordee.
3.In our series there was greater requirement for inferior pubectomy(67%).This was required at essentially the same rate,regardless of whether it was a primary or repeat procedure[3,4].This may be due to anthropometric differences in pelvic bones,penile length and mechanisms ofinjury in patients from different ethnic backgrounds[5-7].Majority of cases referred to our institute did not have inferior pubectomy and this may have led to the failure of the procedure.
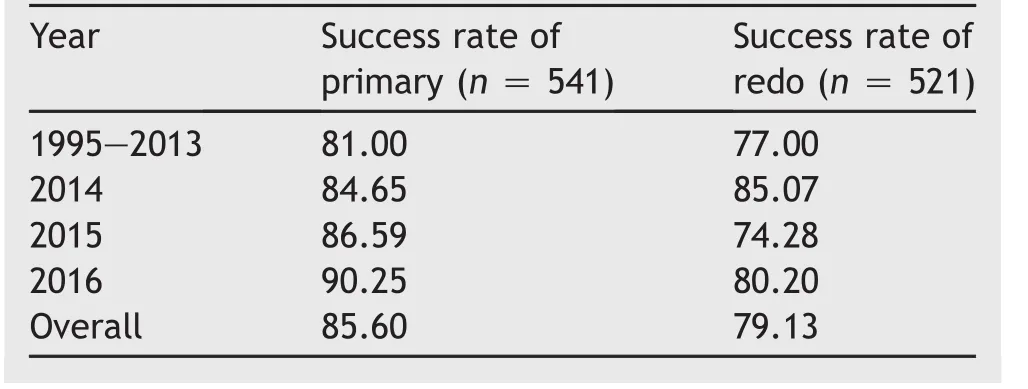
Table 1 Success rate of primary vs.redo urethroplasty(%).
Fig.2B demonstrated the typical findings on RGU and VCUG in complex PFUI.
Tips for redo anastomotic urethroplasty for PFUI:
1.A mastoid retractor is useful for retracting the bulbospongiosus muscle(Fig.2C).
2.Dissect thebulbar urethratill thepenoscrotal junction.A finger is placed between the dissected urethra and corpora with penis in stretched position toidentifythepenoscrotal junction(Fig.2D).Dissection distal to penoscrotal junction will lead to chordee and should be avoided.The concept of limiting dissection till the suspensory ligament is not feasible,as this is not seen during the surgical dissection.
3.Babcock’s forceps should be applied and bulb lifted upwards from the perineal body to facilitate dissection(Fig.2E).
4.At times a retrograde bougie or a flexible cystoscope passed through the SPC tract may not be felt in the perineum.In such a situation,inserting the index finger in the rectum helps locate the bougie at the apex of posterior urethra.This manoeuvre guides the direction of dissection.With the assistant holding the bougie,the surgeon has the index finger of one hand in the rectum while using the operating hand to perform sharp dissection through scar tissue and incise the posterior urethra over the bougie(Fig.2F).
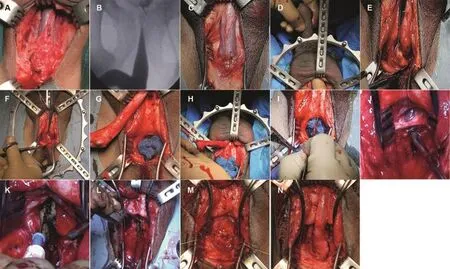
Figure 2 Steps of anastomotic urethroplasty.(A)Distal area shows normal tissue signifying that bulbar urethra was not mobilized in previous surgery until penoscrotal junction;(B)RGU MCU showing high bladder and posterior urethra-complex PFUI;(C)Mastoid retractor applied to retract bulbospongiosus muscle;(D)Finger passed between urethra and corpora in stretched penis to locate penoscrotal junction,which marks upper limit of bulbar mobilization;(E)Use of Babcock’s forceps to lift bulbar urethra;(F)Dissection of bulb with finger in rectum finger in rectum;(G)Accurate transection at level of block to prevent urethral loss;(H)Retrograde bleeding;(I)Knife used to perform crural separation;(J)Preservation of dorsal vein;(K)Periosteal elevation using bent electrocautery tip;(L)Inferior pubectomy;(M)Membranous urethra is not spatulated.Mastoid retractor applied in reverse way to facilitate crural separation.Dorsal penile vein is seen retracted to left corpora;(N)Tension free bulbo membranous anastomosis.RGU,retrograde urethrography;MCU,micturating cysto urethrogram;PFUI,pelvic fracture urethral injuries.
5.The prostatic urethra occasionally gets opened on its anterior wall.A right-angled clamp(Mixter forceps)is passed hugging the posterior wall through the open urethra and incised till the apex(Fig.2G).
6.Intraoperative endoscopy is essential to ensure that the posterior urethra is incised at the correct location and to assess the integrity of bladder neck(Fig.2H).
7.The corpora cavernosa is attached to each other in the midline.A knife(fits well between the two convex cylinders)can be used for initial dissection followed by a blunt scissors for crural separation.Electrodissection should be avoided.An upside down placed mastoid retractor can be used to facilitate further crural separation(Fig.2I).
8.Deep dorsal vein is usually retracted to one side(Fig.2J).Occasionallyit maybeligatedand transected.
9.For inferior pubectomy the periosteum is incised in midline.A bent tip of electrocautery facilitates easy periosteal elevation(Fig.2K).This also avoids inadvertent injury to deep dorsal arteries,which are lateral to the dorsal vein.
10.Pubectomy should be wide enough to accommodate index finger of the operating surgeon.This would allow easy manoeuvring of the needle holder for anastomosis(Fig.2L).
11.Spatulation of the sphincter active membranous urethra is avoided(Fig.2M).
12.Tension free anastomosis is mandatory(Fig.2N).
13.Two ancillary steps that help in reducing tension are pulling the bulbar urethra down and suturing to adjacent corpora or corporal shortening using nonabsorbable sutures.
3.2.Ischemic narrowing or necrosis of bulbar urethra after primary repair
Anastomotic urethroplasty involves transection of bulbar urethra at the level of the block.This compromises blood supply from the bulbourethral arteries.Circumferential mobilization of the bulbar urethra involves coagulating the circumflex vessels and perforators.The anterior urethra is now dependent only on retrograde blood flow from glans and dorsal penile artery.Patients with poor retrograde blood flow develop ischemia of this mobilized bulbar urethra,which can manifest as necrosis(Fig.3A)or complete loss resulting in bulbar stenosis(Fig.3B).
This condition was labelled as “long gaps” or “unsalvageable”after prior failed urethroplasty[8,9].Turner-Warwick(1986)defined spongionecrosis of the bulbar urethra[10].He described three situations that can lead to spongionecrosis:i)Over mobilisation of distal urethra,ii)concomitant hypospadias,and iii)extensive spongiofibrosis resulting from multiple previous surgeries.
After crural separation the dorsal penile vein is identified in the midline.Lateral to it are the dorsal penile arteries.Our theory is that if the periosteum is not elevated at inferior pubectomy or due to improper technique of pubectomy there can be damage to these dorsal penile arteries,which leads to poor retrograde flow.We routinely perform preoperative penile doppler to evaluate the flow in dorsal penile arteries.Patients with this complex problem require vascularized flaps for augmentation(in stenosis)or substitution(in necrosis).
Specific procedures performed for this condition,in our institution,include:
1.Pedicled preputial tube:Inner circumcision incision is performed deep to dartos and outer circumcision incision is performed deep to skin but superficial to dartos.As a result,the prepuce is mobilized based on dartos pedicle.It is incised ventrally and transposed to perineum,tubularised and substitution urethroplasty performed(Fig.3C-3G).
2.Oral mucosal flap:We developed this technique in patients who had prior circumcision and bulbar necrosis.In first stage an incision is made on the scrotum in the midline.A 7 cm×3 cm wide buccal graft is place and quilted on dartos(Fig.3H).The graft is reassessed.After 2-4 weeks it derives vascularity from underlying dartos of the midline scrotal septum.It is mobilized on the dartos pedicle,transposed to perineum and then used as onlay flap or tubularised.Thus,a graft can be converted to flap(Fig.3I and 3J).
3.Scrotal drop back(Turner-Warwick)
4.Pedicled penile skin flap(Q flap and McAninch Flap)in cases where prepuce is absent(Fig.3C-3G).
5.Enterourethroplasty.We have performed two enterourethroplasties as described by Mundy and Andrich[9]using sigmoid colon.Both patients are voiding well without need for any dilatation(Fig.3K and 3L).
6.Use of buccal mucosa graft(BMG)dorsally and flap ventrally.This can be performed and provided inferior pubectomy is not required.An intact corpora positioned in the midline is required to quilt BMG.
7.Pedicled anterolateral thigh flap for reconstruction for urethral defects[11].
8.Forearm flap with micro vascular anastomosis to inferior epigastric artery[12].
9.Dorsal BMG with ventral BMG on gracilis muscle[13].
The details of success rate as per choice of management have been highlighted in Table 2.
Use of skin flaps can lead to diverticulum formation,which may later need reduction urethroplasty.Hence the urine flow may not always show a bell-shaped curve.Average urine flow in our study in cases where skin flaps were used was 10.5 mL/s(3-26 mL/s).The pedicled preputial tube acts as a conduit but does not have viscoelastic properties of normal urethra.
Our success rate to treating bulbar necrosis was 76.67%.
3.3.Boys aged<12 years
PFUI in young boys is challenging due to two factors-long gap and small urethral size.Flynn et al.[14]in their study of prepubescent boys reported that redo repair required more elaborate procedures,and that the vascular connections in the glans were insufficient,resulting in a suboptimal retrograde blood flow.Similar injuries to the posterior urethra in an adult are less devastating than in children owning to the underdeveloped prostate.Hence,the best chance of success is at the first repair.Urethral disruptions in children can occur anywhere from the bladder neck through the entire posterior urethra compared to adults where the injury is usually at the bulbomembranous junction.Common sites ofinjury in children include supraprostatic,transprostatic,prostatomembranous,and bulbomembranous junction[15].In children the repair is difficult due to the high incidence(44%)of proximal dislocation of the prostate due to shearing of puboprostatic ligaments by sudden displacement of the fractured pubic rami[16].The anatomical differences in children must be borne in mind when evaluating RUG,VCUG and making decisions on surgical reconstruction.
Sixty-six patients aged<12 years were retrospectively reviewed.The mean age at the time of repair was 9.2 years(1-12 years)and mean follow-up was 43 months(12-240 months).In all cases,road traffic accident was the cause for pelvic fracture.All patients presented with a suprapubic catheter.Twenty-six of the 66 children were redo cases while 40 had a primary repair.
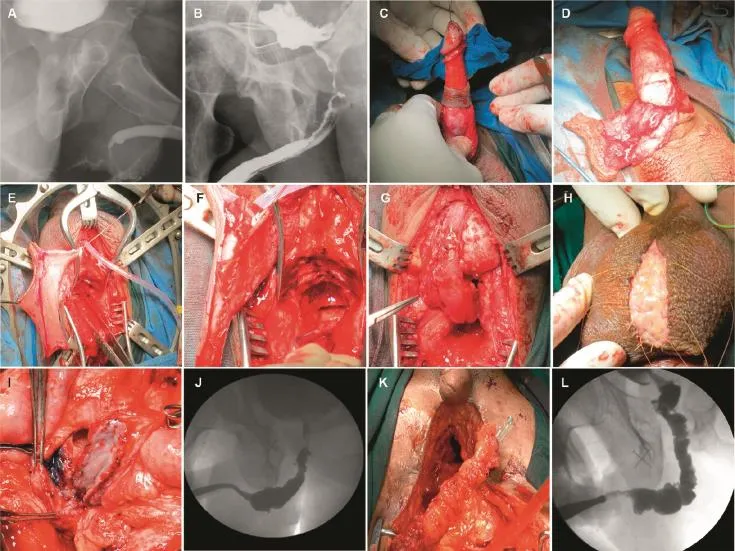
Figure 3 Bulbar urethral necrosis.(A)RGU showing bulbar urethral necrosis;(B)RGU showing bulbar urethral stenosis;(C)Inner and outer circumcision for pedicled preputial flap;(D)Pedicled preputial flap based on dartos;(E)Preputial flap transposed to perineum;(F)Flap tubularised on a catheter;(G)Pedicled preputial flap based on dartos pedicle used as tubularised substitution urethroplasty;(H)BMG applied on scrotum in first stage;(I)BMG mobilized on midline scrotal incision and the oral mucosa flap is applied as dorsal onlay to the stenosed urethra;(J)RGU showing BMG flap in another patient where it was tubularised as substitution urethroplasty;(K)Sigmoid colon tubularised:Enterourethroplasty pedicle of prepucial flap;(L)RGU of a patient with enterourethroplasty.BMG,buccal mucosa graft;RGU,retrograde urethrography.
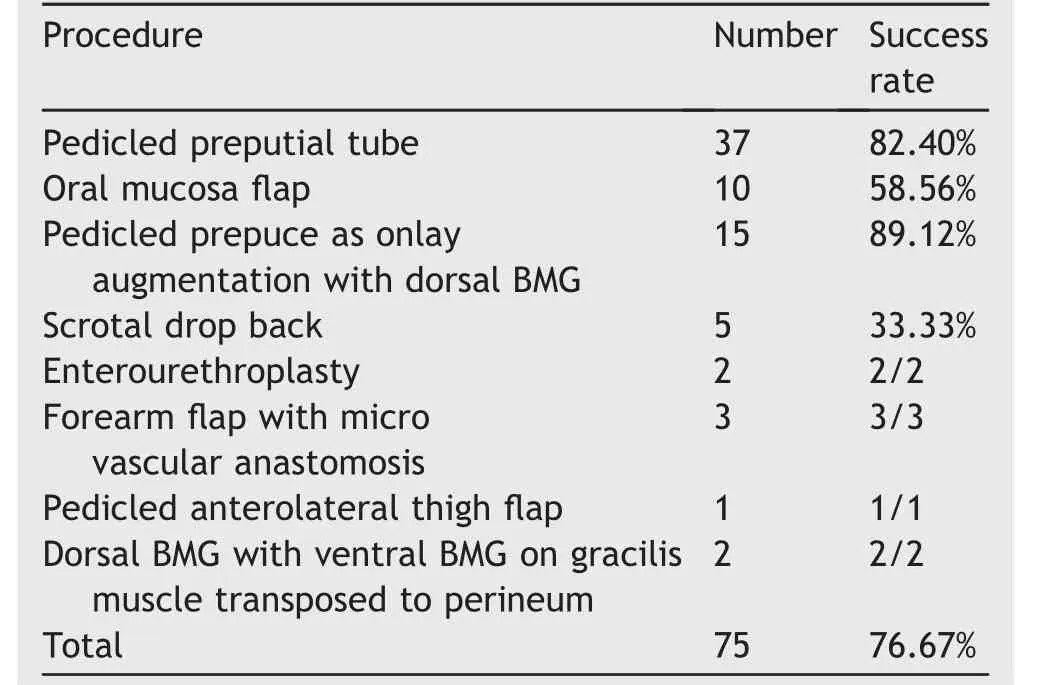
Table 2 Bulbar urethral necrosis/stenosis-management and success rate.
A standard perineal approach was attempted with use of elaborated and transpubic approach in those where perineal repair is not possible(Fig.4A and 4B).Transpubic/abdominal approach was required in 31%of the time,compared to 9%in adults.We perform a posterior pubectomy in our transpubic approach,leaving a rim of anterior pubic bone intact.This avoids gait complications and herniation due to complete disruption of the pelvic ring.
We could perform the anastomosis using crural separation in only 14%cases,compared to 22%in adult patients.The bulbar urethra in children has yet to develop fibroelastic properties,and as such a simple bulbar mobilization is unlikely to provide the length required for tension-free repair.
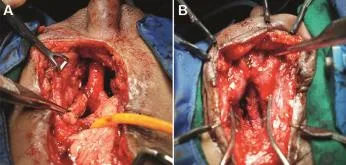
Figure 4 (A)Transpubic urethroplasty with omental wrap in a child with pelvic fracture urethral injuries(PFUI);(B)Step 4-Supracrural rerouting in a child with PFUI.
3.4.Girls aged<12 years with associated urethrovaginal fistula
PFUI in females is rare.Two reviews reported the incidence of PFUI in females as high as 4%-6%with increased incidence in young girls compared to adult females[17,18].In our experience,road traffic accident has been the commonest aetiology of PFUI in females.Most injuries get missed at initial assessment emphasizing the need for careful diagnostic evaluation.The injury can be at the level of the bladder neck,proximal,mid or distal urethra.
We treated nine young girls and five adult females with PFUI at our centre.Adult females were excluded from this review.Management of young girls is challenging,as transvaginal surgery is not possible or challenging.All of them required an abdominal approach.
Preoperative surgical planning requires VCUG and pelvic MRI.We found that the distal urethra was usually communicating with vagina as a urethrovaginal fistula and needs to be delineated intraoperatively.Antegrade cystoscopy is useful in assessing the bladder neck.Vaginoscopy and distal urethroscopy was performed to identify the urethrovaginal fistula.Urethral transection was proximal in two girls and mid-urethral in five girls.Standard steps included identifying the bladder and a posterior pubectomy(Fig.5B).A bougie was then passed through the SPC tract and the blocked urethra opened.A guide wire passed from the distal urethra to the vagina was identified(Fig.5C).Vaginal opening was closed and omentum interposed between urethra and vagina.The urethral ends were anastomosed over a perurethral Foleycatheter(Fig.5D).Five girls had a successful outcome while one required redo surgery and one required dilatation of urethra(Table 3).
We had two girls and one adult female in whom the injury was at the level of the vaginal introitus(Fig.5A).There was distal urethral injury leading to loss of urethra and a hypospadiac urethral meatus opening in the anterior wall of vagina.The presenting symptom was continuous dribbling of urine from the vagina.Careful examination revealed an obliterated vaginal introitus.The vaginal orifice was dilated over a guide wire and lateral episiotomy was performed.The SPC was removed and the females had normal voiding from the hypospadias meatus.However,after an interval of 3-4 months the introitus narrowedagainrequiringfurtherdilatations.After consultation with gynaecology peers,it was decided to consider a formal vaginal repair at a later age as vagina was small at the time of our repair.These girls were on repeated periodic vaginal dilatation but were continent and free of catheters.
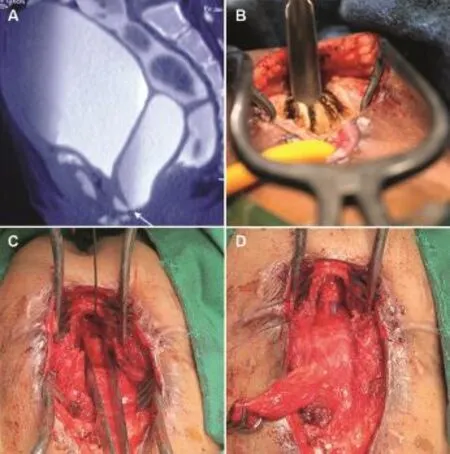
Figure 5 PFUI in girls and females.(A)MRI of a girl with vaginal and urethral stenosis and urine in vagina;(B)Posterior pubectomy in a girl with pelvic fracture urethral injuries(PFUI);(C)Distal urethra with forceps in vagina fistula after disconnection of urethra vaginal fistula;(D)Urethral anastomosis.Omentum was seen being held by the Babcock’s forceps.
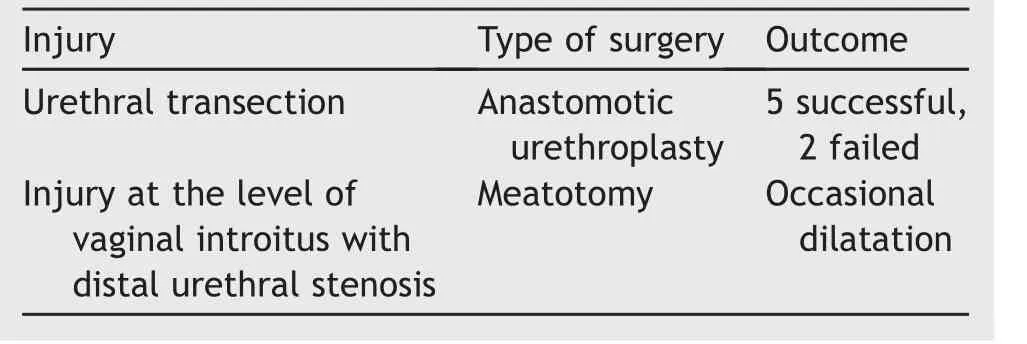
Table 3 Female pelvic fracture urethral injuries management.
One adolescent female had successful anastomotic urethroplasty with repair of urethrovaginal fistula using standard steps mentioned above.However,she developed hematocolposonachievingmenarche.Examination revealed a transverse vaginal septum with scar most probably due to primary injury in childhood.She underwent vaginal repair and is now relieved of her symptoms.
3.5.Double block at bulbomembranous junction and bladder neck-prostate
Injury in PFUI is usually at membranobulbar junction.Uncommonly the injury can occur at two levels-bladder neck-prostate junction and membranobulbar urethra.Mundy and Andrich[19]reported 15 patients with bladder neck injuries of whom two had a double block at membranobulbar and bladder neck-prostate level.They termed this as a “sequestered prostate”.Kulkarni et al.[3]reported five patients with double block.
These patients are usually identified on a preoperative VCUG and RGU where bladder neck is not identified and posterior urethra does not get delineated.The prostatic urethra gets sequestered and filled with seminal fluid.This appears as a cyst on MRI(Fig.6A).
There are two main issues in managing such patients:
1.High risk ofincontinence as both sphincter mechanisms may sustain injury;
2.In children the prostate is underdeveloped and needs meticulous surgery using optical magnification.
We have treated eight patients with double block(three adults and five children).Initial two patients were incontinent which made us modify our surgical steps to preserve continence mechanism.
Mundy and Andrich[19]in their review found that 85%of patients of PFUI have functioning external urethral sphincter mechanism after successful anastomotic repair.Normally in a standard anastomotic urethroplasty the posterior urethra is identified and incised on a bougie passed through SPC tract or overa flexible cystoscopy.In a double block itisnotpossible as the bladder neck is obliterated.Bladder neck is unlikely to support continence after reconstruction.We identified the membranous urethra and performed an anatomic membrano bulbar anastomosis to maintain continence.
The standard steps in our unit for such cases include:
1.Perineal incision,transection of bulbar urethra at level of block.
2.Abdominal incision,identifying bladder,incising bladder neck over a rigid ureteroscope or bougie passed through SPC.(We avoid median cystostomy.)
3.Excision of scar around the bladder neck and prostate
4.Identifying prostate by inserting a wide bore needle,which would then show efflux of seminal fluid(Fig.6B).Finger in rectum could facilitate identifying the prostate.
5.Guide wire is passed into prostatic urethra and tract dilated.Intraprostatic scopy is performed using a 6 Fr ureteroscope and membranous urethra is identified.
6.Through perineum a needle is passed which is spotted in intraprostatic scopy entering exactly at the apex of membranous urethra as described by Hosseini et al.[20](Fig.6C).
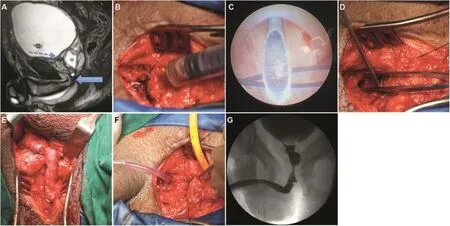
Figure 6 Steps of urethroplasty in patients with double block at bulbo membranous urethra and bladder neck prostate junction.(A)MRI of a child with double block at bladder neck-prostate junction and prostato-Membranous junction.Prostate filled with semen appeared like a cyst;(B)Abdominal approach.Needle was inserted and Seminal fluid was aspirated to locate the sequestered prostate;(C)Needle inserted through perineum was seen coming exactly at membranous urethra seen through intraprostatic scopy;(D)Abdominal approach.Forceps showed base of prostate and suction was inserted at bladder neck;(E)Bulbo membranous anastomosis through perineum;(F)In preparation for prostate vesical anastomosis;(G)Follow-up RGU.RGU,retrograde urethrography.
7.Spatulation of bulbar urethra,no spatulation of membranous urethra and anatomic bulbomembranous anastomosis(Fig.6D and 6E).
8.Bladder neck-prostate anastomosis with omental wrap(Fig.6F).
Using this technique ofintraprostatic endoscopy and identification of membranous urethra the remaining one adult and five children are continent.Three children have mild degree of nocturnal enuresis.The adult patient is potent,has normal ejaculation and normal urine flow(Fig.6G).The incontinent adult awaits insertion of artificial urinary sphincter.
3.6.Recto urethral fistula(RUF)
Management of RUfis challenging.This usually occurs due to crush or penetrating trauma to the rectum and perineum[21].Patients are usually referred with SPC and diverting colostomy after initial management at trauma centres.Occasionally rectourethral fistula can be iatrogenic(prior attempt at urethroplasty).In a review of 573 patients with a pelvic fracture,Fu et al.[22]identified an iatrogenic injury to the rectum in 5%of cases.These were repaired primarily,with no fistula,but it highlights the risk of RUfin an unrecognized injury from PFUI management.
Surgery for RUfis performed in three steps:
1.Diverting colostomy(usually performedat primary trauma centre).
2.Delayed urethroplasty with closure of RUF.
3.Colostomy closure.
There are two main challenges in management of such patients.
1.There may be rectal stenosis and therefore identifying prostate by inserting a finger in the rectum can be difficult.On many occasions the posterior urethra is high and deep in the pelvis.
2.Patients may develop rectal stenosis or faecal incontinence due to primary injury and then further rehabilitation with closure of colostomy becomes tricky.
In our centre we have performed surgery on 13 patients with PFUI and RUF.In 10 patients primary injury caused RUF while in three patients the aetiology was iatrogenic.Presenting symptoms were fecaluria or voiding through the rectum.
Preoperative VCUG,RGU and MRI were performed to identifythefistuloustract(Fig.7A).Intraoperative cystoscopy was performed to identify the fistula.Guide wire was passed through the fistula and brought out though the rectum.A midline perineal incision was made,bulbar urethra mobilized and transected,fistula identified and excised.Rectum was closed in two layers and anastomotic urethroplasty was performed(Fig.7B).
We have used gracilis(n=3),surrounding perineal fat(akin to Martius pad of fat)(n=4)and one limb of bulbospongiosus(n=2)muscle as vascular intervening tissue.However,a major advancement has been our technique of laparoscopic omentoplasty wherein omentum was transferred to the perineum avoiding a transpubic approach[23](Fig.7C and 7D).Out of 13 patients one patient had normal urethra with iatrogenic RUF.He was treated using a half-moon incision around anal canal(9-3 o’clock)avoiding urethral transection.
Eleven patients were cured at first attempt and two required redo surgery.Nine patients underwent closure of colostomy.In two patients with rectal stenosis,an anal pull through surgery had been performed and patients were on regular self-anal dilatation awaiting colostomy closure.Two Patients with lax anal sphincter underwent MRI of pelvis and were referred to colorectal surgery colleagues for further management.
Our results showed that traumatic urethrorectal fistula in the context of pelvic fracture can be managed via a perineal approach.This can avoid complications encountered on using a perianal/posterior sagittal approach.
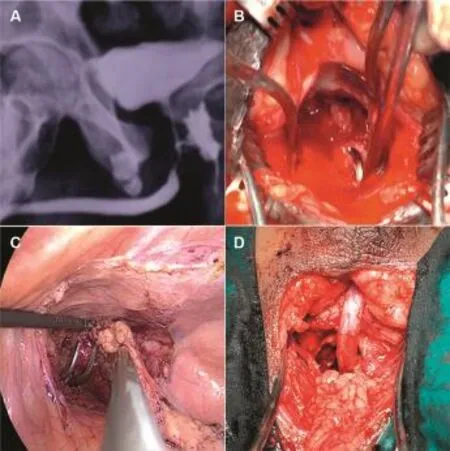
Figure 7 Laparosocpic omentoplasty in patients with recto urethral fistula.(A)RGU showing recto urethral fistula;(B)Right angled clamp passed from rectum through the RUF.The fistula was closed;(C)Right angled clamp was passed from perineum in to the retroperitoneum space lateral to bladder as seen in simultaneous laparoscopy.The mobilised omentum was transposed to perineum laparoscopically;(D)Laparoscopic omentoplasty as interposition flap in RUF.RGU,retrograde urethrography;RUF,Recto urethral fistula.
3.7.Incontinence due to bladder neck injury
Injury in PFUI was initially thought to be membranoprostatic.It was assumed that continence was dependent on preserved bladder neck.Andrich and Mundy[24]in their review found that 85%of patients of PFUI had functioning external urethral sphincter mechanism after successful anastomotic repair.In those where the injury is membranous,continence primarily depends on bladder neck sphincter mechanism.We performed preoperative antegrade cystoscopy through the SPC tract to assess the bladder neck visually.
There were three types of bladder neck function after PFUI:
1.Patients who had closed bladder neck can be assumed to have normal function postoperatively.
2.A wide-open bladder neck was seen at rest,during cystography(Fig.8A)and antegrade cystoscopy(possibly due to neuropraxia).If the membranous urethra was intact and meticulous bulbo-membranous anastomosis was performed,then such patients can remain continent after a successful anastomotic urethroplasty[25].Preoperative patient education and counselling regarding the risk ofincontinence was of paramount importance.
We had two patients who had membranous injury with neurogenicinjuryaffectingthebladder neck.They required an artificial urinary sphincter.
3.A tear drop deformity at 12 o’clock was seen where there was trauma to bladder neck.Usually this is due to a fragment of the fractured pubic bone impinging on the bladder neck(Fig.8B and 8C).
We had three patients who had a tear drop deformity of the bladder neck resulting in incontinence.Surgical management includedanabdominal approachwith midline cystostomy.The incision was extended across the bladder neckintotheprostaticurethra.Scar at the bladder neck was excised.Bladder neck was closed around periurethral Foleys catheter.Bony fragment of the pubic bone if present was excised.Two patients are continentandonewasawaitingartificial urinary sphincter insertion.
Turner-Warwick described that scar around the bladder neck prevents it from closing.We have performed scar removal and wrapping of bladder neck with omentum.However,this procedure has not yielded favourable results.Such patients should be considered for artificial urinary sphincters.In our experience only patients with tear drop deformity of anterior bladder neck benefit from bladder neck reconstruction.
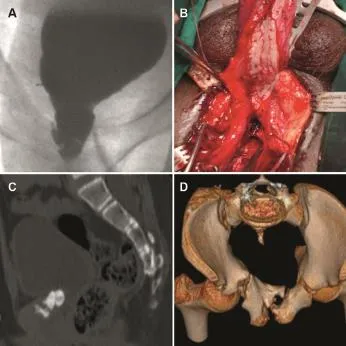
Figure 8 (A)Open bladder neck in pelvic fracture urethral injuries(PFUI);(B)Combined anterior with posterior urethroplasty;(C)3D CT reconstruction showing bone chip indenting the bladder neck;(C)and(D)3D CT reconstruction showing bone chip indenting the bladder neck.
3.8.Patient who have concomitant posterior urethral injury with anterior urethral strictures
Amongst 1062 patients seven patients had anterior urethral strictures along with PFUI.Details of the patients have been mentioned in Table 4.
The anterior urethral strictures urethra were bulbar,penile or panurethral.The cause of anterior urethral stricture was iatrogenic due to multiple attempts at catheterization at initial injury or multiple endoscopies.There remains a dilemma as to which stricture should be treated first and by what approach.Only one paper exists in literature describing management of such strictures.However,the authors used dilatation for more than 50%of patients with a failure rate of 44%[26].A staged urethroplasty has been performed in majority of cases.
An approach preserving the blood supply to the anterior urethra should be used.Management of PFUI requires transection of bulbar urethra at level of block.This leads to transection of bulbourethral arteries.The bulbar urethra now depends on retrograde flow from glans and circum flex flow from dorsal penile arteries for maintaining the vascularity.
Kulkarni et al.[27]published the technique of onesided dissection for bulbar urethral and panurethral stricture.The urethra is mobilized dorsally across the midline.Circumferential mobilization must be avoided.As a result,the neurovascular tissue on one side(usually right of patient as majority of surgeons are righthanded)remains intact.This is a useful adjunct in managing complex cases of PFUI.Our philosophy has been to perform a single stage anterior with posterior urethroplasty.
Important steps include(Fig.8D):
·One-sided dissection of bulbar urethra,which maintains the lateral neurovascular supply.
·The proximal most bulbar urethra could be transected with minimal mobilization facilitating scar excision.If possible one side bulbourethral artery is preserved.
·Penile invagination with one sided dissection for patients with panurethral stricture.
·Augmentation of anterior urethra with buccal graft depending on location of stricture.
·Bulbo-membranous anastomosis with at least six anastomotic sutures.
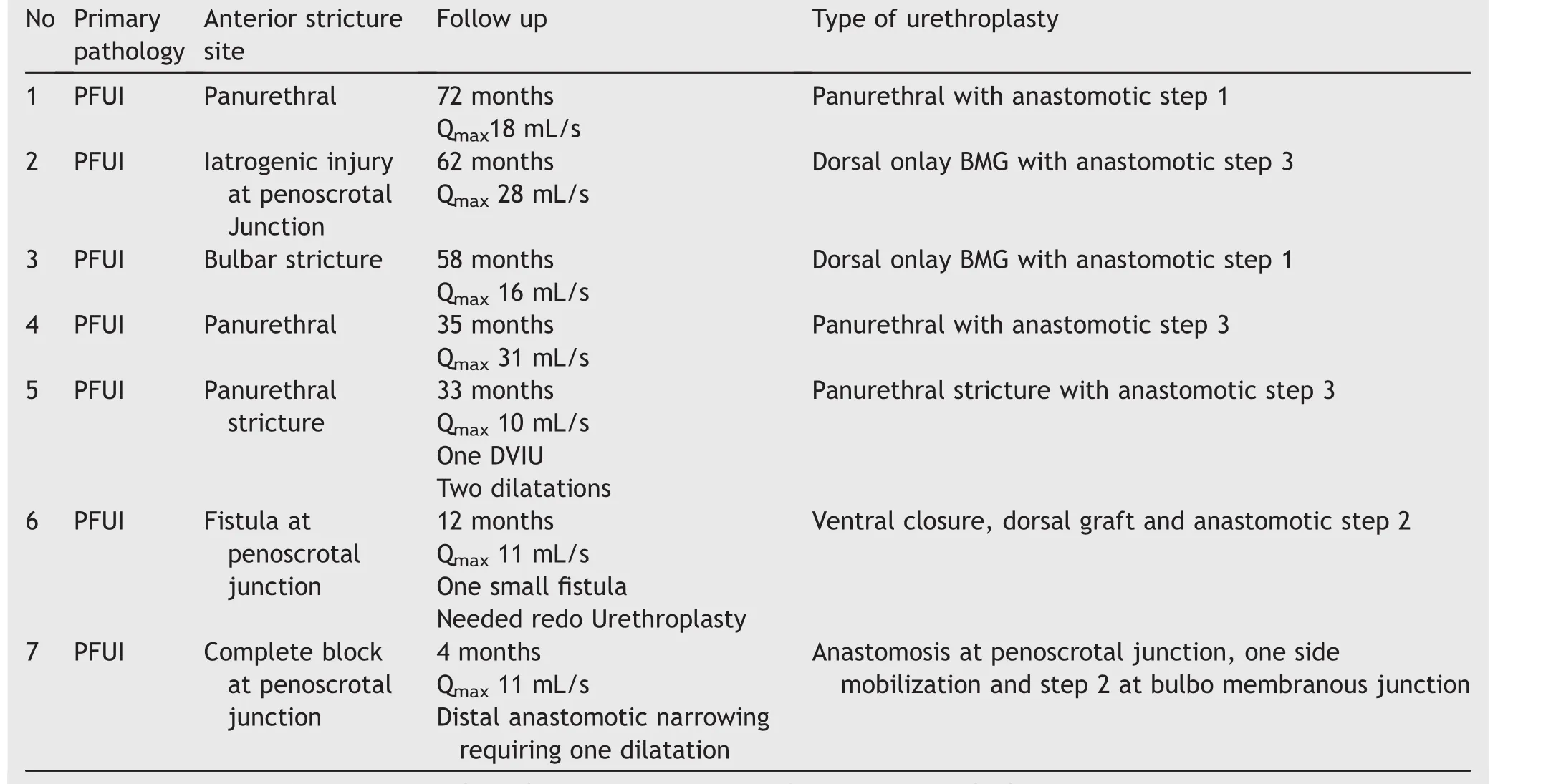
Table 4 Anterior urethral stricture and PFUI.
4.Conclusion
Anastomotic urethroplasty for PFUI should be performed in experienced hands at high volume centres.Successful management of multiple failed urethroplasties includes bulbar urethral mobilization,excision of scar,optimal inferior pubectomy and tension free anastomosis between bulbar and membranous urethra.Ancillary steps described in the article are useful in achieving success in difficult cases.
Young children with PFUI are more likely to need transabdominal approach.Doubleblockat bladder neck-prostate and membrano-bulbar urethra is uncommonbut possible.Identifyingmembranous urethra throughintraprostaticscopyandperformingbulbomembranous anastomosis can preserve continence in such patients.
Anastomotic urethroplasty with use ofintervening tissue is a standardised management for PFUI with rectourethral fistula.Patients with bladder neck incontinence due to teardrop deformity merit anatomic reconstruction.Patients with persistent incontinence after repair or in those with neurogenic cause require insertion of an arti ficial urinary sphincter to achieve continence.Concomitant anterior urethral strictures in patients of PFUI should be treated with vessel preserving single stage simultaneous urethroplasty.
Conflicts ofinterest
The authors declare no conflict ofinterest.
[1]DemetriadesD,KaraiskakisM,ToutouzasK,AloK,Velmahos G,Chan L.Pelvic fractures:epidemiology and predictors of associated abdominal injuries and outcomes.J Am Coll Surg 2002;195:1-10.
[2]Joshi PM,Desai DJ,Shah D,Joshi D,Kulkarni SB.Injury in pelvic fracture urethral injury is membranobulbar:fact or myth.Urology 2017;102:e9-10.
[3]Kulkarni SB,Joshi PM,Hunter C,Surana S,Shahrour W,Alhajeri F.Complex posterior urethral injury.Arab J Urol 2015;13:43-52.
[4]Kulkarni S,Barbagli G,Kulkarni J,Romano G,Lazzeri M.Posteriorurethral strictureafterpelvicfractureurethral distraction defects in developing and developed countries,and choice of surgical technique.J Urol 2010;183:1049-54.
[5]Kizer WS,Armenakas NA,Brandes SB,Cavalcanti AG,Santucci RA,Morey AF.Simplified reconstruction of posterior urethral disruptiondefects:limitedroleof supracrural rerouting.J Urol 2007;177:1378-81.discussion 1381-1382.
[6]Krishnamoorthy V,Joshi PB.Length of urethra in the Indian adult male population.Indian J Urol 2012;28:297-9.
[7]Kohler TS,Yadven M,Manvar A,Liu N,Monga M.The length of the male urethra.Int Braz J Urol 2008;34:451-4.discussion 455-456.
[8]Barbagli G.History and evolution of transpubic urethroplasty:a lesson for young urologists in training.Eur Urol 2007;52:1290-2.
[9]Mundy AR,Andrich DE.Entero-urethroplasty for the salvage of bulbo-membranous stricture disease or trauma.BJU Int 2010;105:1716-20.
[10]Turner-Warwick R.The principles of urethral reconstruction.In:Rob C,Smith R,Scott McDougal W,editors.Rob and smith’s operative surgery,urology.London:Butterworths;1986.p480-519.
[11]Zhe Y,Yangqun L,Yong T,Muxin Z,Wen C,Ning M,et al.The pedicled anterolateral thigh flap for penile reconstruction.Chin J Plast Surg 2015;11:406-10.
[12]Chauhan A,Sham E,Chee J.Microsurgical urethroplasty for complex bulbar urethral strictures using the radial forearm free flap prelaminated with buccal mucosa.J Reconstr Microsurg 2016;32:378-85.
[13]Nikolavsky D.Prelaminated gracilis flap with buccal mucosal graft for salvage of devastated urethra.Case Rep Urol 2015;2015:490518.
[14]Flynn BJ,Delvecchio FC,Webster GD.Perineal repair of pelvic fracture urethral distraction defects:experience in 120 patients during the last 10 years.J Urol 2003;170:1877-80.
[15]Boone TB,Wilson WT,Husmann DA.Postpubertal genitourinary function following posterior urethral disruptions in children.J Urol 1992;148:1232-4.
[16]Koratim MM.Posttraumatic posterior urethral strictures in children:a 20-year experience.J Urol 1997;157:641-5.
[17]Perry MO,Husmann DA.Urethral injuries in female subjects following pelvic fractures.J Urol 1992;147:139-43.
[18]Black PC,Miller EA,Porter JR,Wessells H.Urethral and bladder neck injury associated with pelvic fracture in 25 female patients.J Urol 2006;175:2140-4.
[19]Mundy AR,Andrich DE.Pelvic fracture-related injuries of the bladder neck and prostate:their nature,cause and management.BJU Int 2010;105:1302-8.
[20]Hosseini SJ,Kaviani A,Jabbari M,Hosseini MM,Haji-Mohammadmehdi-Arbab A,Simaei NR.Diagnostic application of flexible cystoscope in pelvic fracture urethral distraction defects.J Urol 2006;3:204-7.
[21]Al-Ali M,Kashmoula D,Saoud IJ.Experience with 30 posttraumatic recto urethral fistulas.Presentation of posterior transsphincteric anterior rectal wall advancement.J Urol 1997;158:421-4.
[22]Fu Q,Zhang J,Sa YL,Jin SB,Xu YM.Recurrence and complications after transperineal bulboprostatic anastomosis for posterior urethral strictures resulting from pelvic fracture:a retrospective study from a urethral referral centre.BJU Int 2013;112:E358-63.
[23]Kulkarni SB,Barbagli G,Joshi PM,Hunter C,Shahrour W,Kulkarni J,et al.Laparoscopic omentoplasty to support anastomotic urethroplasty in complex and redo pelvic fracture urethral defects.Urology 2015;85:1200-5.
[24]Andrich DE,Mundy AR.The nature of urethral injury in cases of pelvic fracture urethral trauma.J Urol 2001;165:1492-5.
[25]Iselin CE,Webster GD.The significance of the open bladder neck associated with pelvic fracture urethral distraction defects.J Urol 1999;162:347-51.
[26]Deng T,Liao B,Luo D,Liu B,Wang K,Liu J,etal.Managementfor the anteriorcombined with posteriorurethralstricture:a 9-year single centre experience.Int J Clin Exp Med 2015;8:3912-23.
[27]Kulkarni S,Kulkarni J,Surana S,Joshi PM.Management of panurethral strictures.Urol Clin North Am.2017;44:67-75.
 Asian Journal of Urology2018年2期
Asian Journal of Urology2018年2期
- Asian Journal of Urology的其它文章
- Tissue engineering for urinary tract reconstruction and repair:Progress and prospect in China
- Overcoming scarring in the urethra:Challenges for tissue engineering
- Emergency treatment of male blunt urethral trauma in China:Outcome of differentmethods in comparison with other countries
- Prevention strategies for ureteral stricture following ureteroscopic lithotripsy
- The association of benign prostatic hyperplasia with lower urinary tract stones in adult men:A retrospective multicenter study
- The effect of adjunct caudal block on postoperative analgesia in robot-assisted laparoscopic radical prostatectomy:A prospective randomized controlled,single blinded pilot study in a tertiary centre
